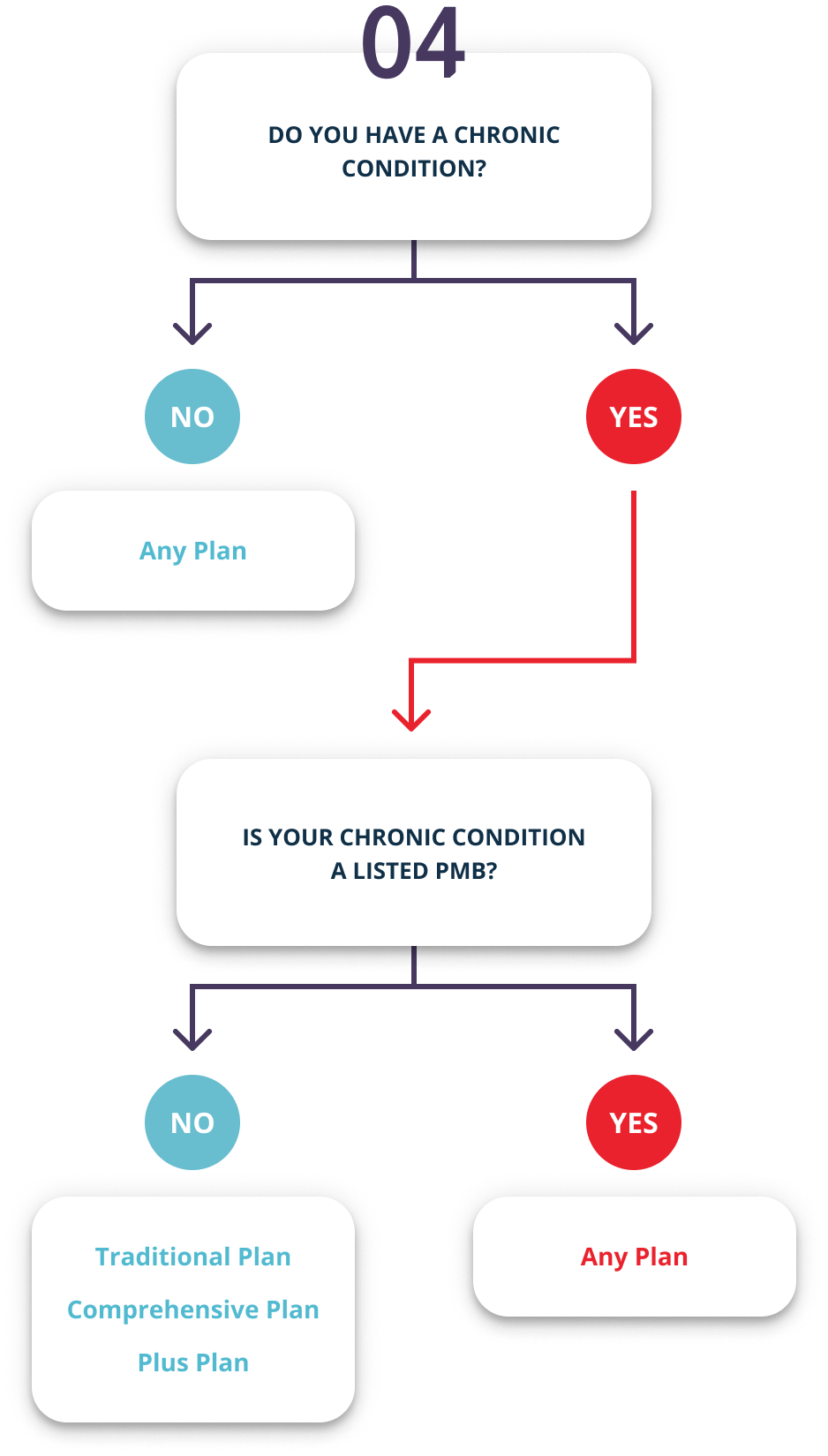
All Bankmed Plans offer cover for chronic conditions that qualify as PMBs on the Chronic Disease List. You must register for the Chronic Illness Benefit to get cover for the medication, tests and treatment you need for your condition.
Chronic Disease List: All Plans
Addison's disease, asthma, bipolar mood disorder, bronchiectasis, cardiac failure, cardiomyopathy, chronic obstructive pulmonary disease, chronic renal disease, coronary artery disease, Crohn's disease, diabetes insipidus, diabetes mellitus types 1 and 2, dysrhythmias, epilepsy, glaucoma, haemophilia, hyperlipidaemia, hypertension, hypothyroidism, HIV and AIDS, multiple sclerosis, Parkinson's disease, rheumatoid arthritis, schizophrenia, systemic lupus erythematosus and ulcerative colitis.
While higher Plans can offer additional cover for these chronic conditions, we pay for specific care (PMBs) for these conditions, no matter which Plan you are on.
Chronic Disease List: Traditional, Comprehensive and Plus Plans
Acne, Attention Deficit Hyperactivity Disorder, Allergic Rhinitis, Anxiety Disorder, Atopic Dermatitis, Alzheimer's disease, Benign Prostatic Hypertrophy, Cardiac Dysrhythmia, Cystic Fibrosis, Gastro Oesophageal Reflux Disease, Gout, Hyperthyroidism, Myasthenia Gravis, Ankylosing Spondylitis / Osteoarthritis, Osteoporosis, Peptic Ulcer Disease, Psoriasis, Schizo-Affective Disorder, Trans Ischaemic Attack, Major Depression, Urinary Incontinence, Menopause, Paraplegia and Stroke.
The Basic Plan covers treatment for Major Depression. The Comprehensive and Plus Plan, covers treatment for Meniere's Disease and Interstitial Lung Fibrosis.